-
- 30
Aug - (0)
Joint Efforts
More often than not, joint EHR implementation efforts have failed.
These days, I’m hearing of more successful Electronic Health Record (EHR) purchase and implementation efforts that include several Mental Health agencies. This is a good thing for professionals and consumers on a variety of levels, not the least of which is accurate recording of treatment history, which paints a picture that may guide both professionals and consumers to more successful treatment and a happier life for the consumer.
 The success is significant because several vendors have attempted to make a big splash by selling a single software implementation to multiple agencies in a geographic area, but it seldom goes anywhere.
The success is significant because several vendors have attempted to make a big splash by selling a single software implementation to multiple agencies in a geographic area, but it seldom goes anywhere. Why is that?
I read an article in Behavioral Healthcare Magazine that tackles this subject, and I can expand on their take.
Lynn Duby, CEO of Crisis and Counseling Centers in Augusta, Maine shared that the five agencies joining together for a software purchase had “strong ties”. That’s tough to develop among competitors, and if there’s no unity, success will be limited. In the past, once a mental health or addiction treatment agency made the decision to buy a certain system from a certain vendor, the implementation often did not go well. The major reason for that is that the customer and vendor were simply not on the same page. When an agency buys an EHR, there are a lot of considerations beside price and whatever the driving force is to buy it now…what about the consumer? If professionals are stumbling through the software’s workflow to find the documents they need to make a point in a session, perform an assessment, or collaborate with the consumer on the treatment plan, the consumer is just sitting there, feeling they are wasting time, or worse, living in their disorder. That’s no fun for anybody, and is bad for business. The solution is to purchase software that works for all the parties involved, and the way to do that is to approach the purchase with a plan that’s been successful elsewhere.
The banding together of five agencies to collaborate on an EHR suddenly becomes much more complicated because they work differently. Sure, the state and federal requirements are the same, but the way professionals work differs from agency to agency…that’s what helps give agencies a personality the consumer can feel when they walk in the door. Duby’s comment about “strong ties” tells us that the software must be flexible enough to suit all five agencies’ workflows for all departments, and the professionals need to be flexible, too, in order to use common electronic documents and make the software affordable…Developing five different treatment plans is pretty expensive compared to making a couple minor adjustments on both the software and professional levels. The professionals who were less-than-enthusiastic about new EHR software either took an active role in the software selection, or developed a very Zen attitude: It is what it is.
It seems to be a fact that decision-making by committee is slower than when a single, strong leader is in the picture. When a number of professionals with different ways of working collaborate on an EHR, the committee becomes the decision-making method. I prefer working with a strong leader (or being one), and there are a lot of strong personalities involved in the management-by-committee scenario. Oftentimes, some of these personalities are at odds with one another and managing conflict becomes a major part of the process. I think it’s a great success when an EHR selection can be made in less than a year. Most either take longer or fizzle out entirely (just to give you an idea, it ought to take 90 days or so).
There are a number of methodologies that can be followed to make the most effective use of time and professional resources in the purchase and implementation of an EHR. Sorting out the acceptable methods for both buying and configuring a software system goes much more smoothly once a specific plan is made, and the committee agrees to stick to the plan. Bringing a number of diverse plans together to hammer out what works for all professionals involved is a chore, but without a commonly accepted plan, likelihood of success is diminished.
If you’re involved in a scenario like this, it’s good to have a professional on hand to guide the committee, whether the group hires a full-time project director or gets guidance from a consultant, success is more likely with a good plan.
Read more → - 30
-
- 23
Aug - (0)
Health Home Technology
The guy living on the street, the hopeless alcoholic/drug addict with other diagnosed problems like depression, schizophrenia, bi-polar disorder and whatever else you can throw into the mix, is about to get better.
.jpg) New York is closing applications for agencies to become Health Homes, which means a bundle of improved treatment solutions to focus on our guy mentioned above are about to hit the field. Health Homes at the base level coordinate care for high-usage consumers. The goal is more focused, knowledgeable team treatment.
New York is closing applications for agencies to become Health Homes, which means a bundle of improved treatment solutions to focus on our guy mentioned above are about to hit the field. Health Homes at the base level coordinate care for high-usage consumers. The goal is more focused, knowledgeable team treatment.Our guy needs help from a number of professionals…His addictions need to be dealt with by special professionals in that treatment field. Additionally, medications need to be prescribed by a psychiatrist for his mental disorders. While we’re treating our high-maintenance consumer, let’s add in a psychologist and perhaps an MSW or two to help him overcome Post Traumatic Stress Disorder (PTSD) and find a place to live.
Since this population of consumers seems to continue on the same loop of treatment, people say “None of it works, so why bother?”
That’s the attitude that propagates the growth of this group of folks who have lost hope. They use a ton of services, and don’t get better. Studies have shown that if concerted efforts to coordinate care are implemented, our guy probably will start to recover from all these problems. OK. Fine. So what’s the problem? We have a community of professionals out there who deal with this sort of thing, Medicaid and Medicare likely will pay for the care, so why aren’t these folks getting better.
The answer may be in communication. Assign a case manager to coordinate care in the treatment community and communicate with professionals involved with the consumer, and you deliver the tools so all the professionals know what else is going on with that consumer. Coordinate and communicate to overcome problems with unknown diagnosis and treatment that can lead to drug interaction problems, conflicting therapies, and so on. If a search of a database of Medicare and Medicaid patients numbers (without names) was performed at every intake, and existing treatment was identified, our guy has a chance of recovering through coordinated, effective treatment. This is of great value to Health Homes in coordinating treatment among professionals.
It took me a while, but this is where Information Technology comes in. Any consumer controls outside access to their health information. I envision a checkbox for each provider in the health home the professional belongs to. The consumer agrees or declines sharing the information. Not perfect, because sometimes we’re dealing with consumer paranoia that keeps those things secret, but hey, we’re trying to help.
Here’s what sorts of information would be available to the professionals’ fingertips once an electronic Health Home network of some sort was settled upon:
.jpg) There are a lot of technological details involved, and IT professionals like me enter the picture to help design and implement the details, but this is as decent a solution. It sure beats faxing paper all over the Health Home network. Regional Health Information Networks (RHIOs) and products like Netsmart’s ConnectCare have a head start on delivering secure access to information like this with consumer approval. The difficulty in IT is not the availability of solutions, it’s modifying professional processes and deploying the solutions, integrating these solutions into existing Electronic Health Records (EHRs).
There are a lot of technological details involved, and IT professionals like me enter the picture to help design and implement the details, but this is as decent a solution. It sure beats faxing paper all over the Health Home network. Regional Health Information Networks (RHIOs) and products like Netsmart’s ConnectCare have a head start on delivering secure access to information like this with consumer approval. The difficulty in IT is not the availability of solutions, it’s modifying professional processes and deploying the solutions, integrating these solutions into existing Electronic Health Records (EHRs). The advice is the same as it was when we were kids: don’t do this in your home without supervision.
Read more → - 23
-
- 09
Aug - (0)
Approaching Electronic Health Record Implementation
“Implementing an EHR may very well be the single largest project you will ever be a part of in your career”.
Believe it. I would add that if your organization’s EHR implementation wasn’t effective, the solution is to take a different look at how it’s done and plan to optimize what you have…read on.
 The statement above came from an announcement of a NIATx presentation I received recently. In the past, the biggest problem standing in the way of effectively and completely implementing an Electronic Health Record (EHR) for Mental Health and Substance Abuse Treatment was a reluctance to spend valuable professionals’ time and energy that’s required to be successful and make the software do what you want it to do. This could apply to any system, really, from a single provider to a large organization with hundreds of users.
The statement above came from an announcement of a NIATx presentation I received recently. In the past, the biggest problem standing in the way of effectively and completely implementing an Electronic Health Record (EHR) for Mental Health and Substance Abuse Treatment was a reluctance to spend valuable professionals’ time and energy that’s required to be successful and make the software do what you want it to do. This could apply to any system, really, from a single provider to a large organization with hundreds of users.There are a number of approaches to getting the same thing done that all revolve around the same thing: Make the software do what the organization needs. I find that if we look at a few elements at a time, and note people who might be appropriate to head up that aspect of the implementation, we’re more likely to have a successful effort than if we try to blast everything out at once, disrupting the work and lives of every professional and treatment of every consumer.
Here are a few ideas to spur some thought, starting with what I think is most important, and then a couple different aspects of the broader view from experts in getting jobs done.
McLeod’s Method: A call this “my” method, simply because it’s part of the system I use.
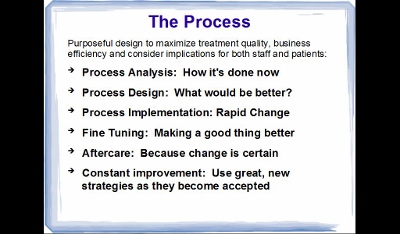 Over the years I’ve picked up a bundle of experience and wisdom from so many sources it would be silly for me to go back and re-construct history….so I call it “mine”. There are many other factors to consider, so I also pay attention to the points attended to by industry leaders in their views below…and more. First, address these bullet points and look into elements like “Rapid-Cycle Change”.
Over the years I’ve picked up a bundle of experience and wisdom from so many sources it would be silly for me to go back and re-construct history….so I call it “mine”. There are many other factors to consider, so I also pay attention to the points attended to by industry leaders in their views below…and more. First, address these bullet points and look into elements like “Rapid-Cycle Change”. Malcomb Baldridge The National Institute of Standards and Technology (NIST) Baldridge Award is a government award for excellence that includes criteria for healthcare for both profit and not for profit organizations. The reason to participate is, according to David Spong, former Boeing executive and winner of the award, is that it improves performance. For professionals, that means not only “production” (seeing more consumers), but improving consumer care for better outcomes. The Baldridge Criteria focus on several elements of importance and help health care organizations achieve and sustain the highest national levels of • Patient safety and loyalty • Health care outcomes • Professional staff satisfaction and engagement • Revenue and market share • Community services
Using the principles and processes of the Baldridge Criteria can’t help but improve an EHR implementation.
NIATx Pointers In a presentation from 2010, NIATx highlighted a number of important points you can use as a guideline in selecting and implementing the EHR. • Why purchase an EHR at all? It may be better for professionals and consumers for the organization to optimize what’s already in place • Is your organization ready? While you’re at it, consider transparency to the consumers and helping them get ready • How do I select a vendor and product? There are tons of approaches: take care, you may want to hire a professional • What about Project Management? Start planning the project prior to purchase so you know what you’re getting into • How does the Implementation affect the entire organization • How do I want to go about training staff and changing business processes to work better for consumers? • What’s the best “Go-Live” strategy? As I’ve said, I’m a big fan of implementing one piece at a time for a bunch of reasons we can talk about later • What are the benefits and problems associated with the EHR implementation?
I don’t mean to sound like a commercial for NIATx, it’s just a good resource. For interested professionals, a NIATx EHR Implementation web presentation is scheduled this week. Given opportunity I plan to listen in, and since I’m a little tardy in posting this, check in with the NIATx website or give them a call to see a copy of the presentation.
Then again, if your organization doesn’t have the people power to manage this sort of effort, and the writing is on the wall that it must be done soon, you may want to consult a professional like yours truly for some help.
Read more → - 09
-
- 29
Jul - (0)
More Services = Healthier Consumers and More Revenue
It only makes sense.
If a professional or professional healthcare team provides a consumer with two services during a visit, the consumer wins because they don’t need to delay getting the help they need and the professional’s revenue increases. I love a win-win scenario.

For the consumer this might mean that a nurse checks her blood pressure, heart rate, etc, and then after a short chat, sends her to a psychologist or other professional to discuss that or another condition. Many apparently physical symptoms like nausea or aches and pains are discovered to be in the realm of a mental health professional’s responsibility; with a root cause of something like grief. This is where an Electronic Health Record (EHR) can really show its stuff in efficiency by electronically alerting other professionals the consumer needs a service and in making sure somebody’s available to help by using the EHR‘s Scheduling Module.
When this sort of thing happens, CFOs love it, process managers love it, and sometimes the treatment professionals may balk at entering a note and charge into the Electronic Health Record (EHR), simply because they’re unsure about the value of that second service and taking the time to record it (some insurance companies and states’ Medicaid won’t pay for the service). We’re all busy people, and it’s possible a second service might not get recorded as an oversight. Today’s EHRs are loaded with reminder systems to make sure scheduled services are addressed, and proper documentation and charges are filed.
Conceivably, since a counseling session can last longer (and pay more) than a short nurse’s visit, only that more profitable service may even make it into the EHR, and therefore the billing system. That could be terribly inconvenient to fostering team spirit, as a professional assigned to diagnosing the patient may want to see the note from the original person who noticed the problem and have a little chat with them before proceeding to treatment for this additional diagnosis. Oh, by the way, depending on who diagnoses the problem and other factors, we may have added to the list another service related to filing the diagnosis itself.
If it’s not in the EHR, the record believes it didn’t happen. It might not be serious, but a secondary service might affect future treatment, so it’s better to record everything.
There are a number of places that second services can be noticed in the EHR, from the front desk checking in, through visits with different professionals, and even at check-out when the consumer gets back to the desk again. A front desk person could notice a limp when a person comes in for a counseling session, or another staff member might notice a consumer with tears in their eyes or who’s behaving oddly. When all staff is mindful about a consumer’s overall health and everybody is acting like a team, more services are rendered. And in the end, even in not-for-profit environments, that can make the difference between replacing somebody who’s left for a different opportunity and giving a salary increase to other staff at the end of the year.
If an organization doesn’t have this sort of mindfulness in place, with the team looking for additional ways a consumer might need help, concentrating on the idea in a staff meeting may be a good idea. Staff education regarding what sorts of symptoms to watch out for can increase vigilance to assure the consumer gets the best care possible. As a bonus to increasing the number of services provided, the revenue of the facility can go up at a time when increasing revenue is critical.
With all that said, there are still operations out there who are stuck with “threshold” billing (where the payor pays one rate for the day, regardless of how many services are provided) for some insurance payors, wherein all services provided during a single day’s visit must be included in that day’s bill for a fixed fee. No extra charge. Others will only pay for explicitly defined additional services under specific conditions. In some cases, payors may seem to make it difficult to charge for additional services. As in anything that has to do with business, you gotta be sharp and make the time it takes to optimize revenue. That may require some help from a consultant or moving a staff member into a position that’s primarily responsible for increasing revenue and assuring documentation and billing are on-track in order to provide the best care possible. With that resource in place, the EHR can be both a guide to making sure needed services are provided to the consumer, and a police officer to assure the billable record is recorded.
Read more → - 29
-
- 19
Jul - (0)
A Facebook Sidebar
On June 21st, I published my comments on Facebook for business…I just didn’t know it had become so important to augment a business site with a Facebook presence. Now I know. Interestingly, the visits to my website jumped by fifty percent for the month. I believe that was simply because Facebook is so doggone popular and my blog came up in the search engines more.

I recently attended the NIATx conference in Boston, and H Westley Clark, Director of CSAT (http://www.samhsa.gov/about/csat.aspx) was a featured speaker. He mentioned in his address that one of the difficulties in delivering treatment documentation to consumers is that it may end up on Facebook. This brings up aspects of confidentiality that are important not only to the consumer, but also to the professional and even the organization they work for.
The Electronic Health Record (EHR) is becoming more and more expansive these days. In addition to the assessments, treatment plans and progress notes, you might see brain scans or even recordings of telemedicine sessions. I asked Jim Mountain, a vendor of telemedicine software, about recording sessions. He advised that it can certainly be done, however, would a professional want to do to that when there’s a danger it could end up on YouTube? All the systems I’ve seen (and I’ve seen a ton) have proven secure, and hackers are not likely to effectively plumb for health information, however, all health records are available to consumers, who might make a decision to share portions of the record on social media. If you’re a professional, consider how you’d feel if your notes were shared that way, or your sessions broadcast.
I believe the consumer’s health record is their property as much as the professionals and the organization they work for. It needs to be guarded, and is. A friend of mine manages a business that protects the consumer identity of methadone treatment recipients from the state…42 CFR prohibits even the state from knowing the identity of consumers they are paying for with Medicaid. The point of this is protection. It’s pretty good these days as long as records aren’t accessed on a lost laptop computer or published on Facebook or YouTube. I doubt it’s likely to happen, but it could. Perhaps an agreement between the consumer and the professional to keep the record that’s provided to the consumer confidential is in order.
This is a huge issue. A couple years ago, Duke FUQUA School of Business published their take on just how huge it is. And they’re not the only ones who’ve been debating, just search of the web on this subject, and you’ll find no shortage of opinions.
This is great food for thought about security, and while the consumer’s privacy is paramount in the business of mental health and substance abuse treatment, it seems to me that the professional’s privacy deserves some respect. And I think that’s the point, professionals spend a considerable amount of time and energy learning their craft, and the subtleties of what they do may be lost on a casual reader, followed by misconceptions that could affect the professional’s business or reputation.
I found these revelations fascinating comments on how our world is changing and Facebook is taking over the world. It will be interesting to watch this issue escalate.
Read more → - 19
-
- 13
Jul - (0)
Enterprise Software Evils
A post on Linked In shared a consultant’s opinion that enterprise software breeds evil.
Well, now, that’s just nonsense. Enterprise software is designed for an agency, in my interest an Electronic Health Record (EHR) for mental health or substance abuse treatment organization, and the software helps people get their jobs done, meet regulatory requirements, assure billing gets done so everybody gets paid, and another very important thing. It may be tempting to rely on memory of a case record rather than go to the chart room to review the consumer’s chart prior to a session. That can be not-so-good; the EHR eliminates trips to the chart room to see previous assessments, progress notes and treatment plans, conceivably bringing a more educated professional into a session and improving the consumer’s likelihood of getting better.
Where does this perception of enterprise software’s evils originate? If I rely purely on anecdotal information, it comes from the customer’s experience with poor implementations. I’ve implemented, been cursorily involved with, and heard of a few EHR implementations, where not every person on the team followed all the advice that ultimately has the professional/consumer relationship in mind. And that shortcoming includes both vendor and agency. Poor planning is the usual culprit.
Over the weekend I went to scenic Boston, MA and attended the NIATx/SAAS conference and was able to sit in on a couple consultants’ sessions about implementing EHRs. I also talked with several vendors, and made an interesting discovery. The “middle tier” of software vendors has come of age. These are software companies that aren’t so big that they’re priced out of a medium-sized agency’s market, or so small they can’t support what they sell. I was particularly interested in the address by keynote speaker David Spong. Another speaker that held my attention was an old friend to substance abuse, H Westley Clark, the director of the Center for Substance Abuse Treatment (CSAT). The consultant’s sessions were interesting insomuch as the questions coming from the audience were the same questions professionals were asking fifteen years ago and before. • How do we pick a software company when there are over 100 vendors out there manufacturing EHRs? • Once we pick an enterprise system, how do we install the doggone software in less than a year and a half? • How do we get professionals to use the system (some are pretty resistant)?
The vendors I talked with in the display area were cordial, very nice guys. I wanted some information that’s key to my business, as it had been a year since I’d updated my records on these vendors. I asked some simple questions, including: • How long have you survived in this tough business? • How many customers do you have, in how many states? • Is your software certified to meet Meaningful Use requirements?
There were more questions, and I plan to address these industry concerns in upcoming posts. Who knows, I may even include some actual information on how to avoid implementation pitfalls and make the experience transparent to consumers…techie consumers are likely to be the only ones interested in this, but for professionals, I think it’s a good subject. I’m thinking about a few reviews of vendors, and sharing my process for narrowing the field of vendors to a manageable few that can be included in a software search.
All in all, the NIATx/SAAS event is a good experience, filled with people who actually care enough about the consumers to stay in business and serve them. I’ll likely attend next time.
…and I software and vendors aren’t evil.
Read more → - 13
-
- 05
Jul - (0)
Feeling the Squeeze
Is treatment quality dropping because of requirements to use the Electronic Health Record (EHR)?
Professionals who hang their own shingle already know that you gotta do the paperwork. If they don’t keep their assessments, treatment plans and notes up to date, they may not be able to bill a consumer’s insurance. Another reason to keep up with the paperwork is that in these documents lie solutions to mental health and addictions problems.
Those working exclusively for agencies may resist spending the time on the paperwork, and that hurts billing, which hurts the paycheck and the organization they work for. Since it’s a key to the paycheck, why do some professionals persist, buying into this old problem and have trouble keeping up with the paperwork?
Lately I’ve been working with a moderately resistant staff that has taken a while to acclimate to using the EHR. After months of work, the professionals are writing the notes to chronicle short, significant activities with consumers that were not previously required. Consumers’ records are up to date and include the new documentation requirements, and billing is on target.
The objective for performance in this particular clinic was determined by analyzing what needed to be done to reach the revenue that would enable the clinic to survive. We discovered a couple interesting things.
All the work was being done before the mandate to record the notes in the EHR became critical (in this case, the progress note triggers a record to the billing system to bill for the consumer’s treatment). Staff felt they didn’t have time to write the notes for these short sessions. They felt the longer sessions were where the meat of treatment was found and really the important thing to document. Were morsels of these shorter sessions ever lost? Who knows. The fact is, they are not lost now.
Prior to the requirement to use the EHR’s progress note to kick off the bill for the session, you might have seen professionals reading the paper or balancing their checkbook in their downtime. No more.
The other day a friend I’ve been working with on this project told me she was pleased with staff’s performance in getting the notes done, and the charges for this work they’ve always performed with consumers, but never been paid for.
There may be a downside.
This clinic, like a lot of clinics, tries to engender a “family atmosphere”. The staff members are all caring professionals, well trained in helping people. My friend’s fear is that their attention to this aspect of the clinic identity is slipping, and consumer treatment may decline in quality. Staff is focused on survival of the clinic. They feel that without writing a ton more short notes to generate more revenue, their jobs may be in jeopardy. So, the solution to this is to broaden attention to include consumer treatment, while still writing a ton more notes. A management issue that may be a constant companion for a while.
To put it simply, this is just a matter of getting used to a new way of doing business. Right now, it may be true that the staff is taking the paperwork and billing quite seriously, perhaps too seriously. I said earlier they are “caring professionals”. As such, they can’t help but help the consumer.
My guess is it just takes time and attention to the details.
Read more → - 05
-
- 13
Jun - (0)
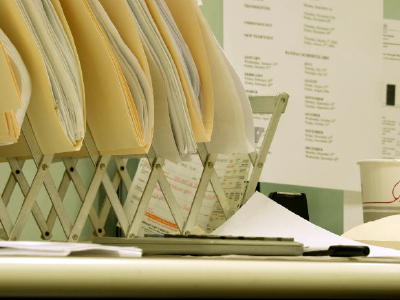
Document Image Management
Boy…that sounds boring.
I suppose it could be for those not interested in the Electronic Health Record (EHR), and for those who are interested, innovations to what Document Management is, its value in treatment, and what it could mean in the future, this is a pretty good topic. Consumers and professionals need to be aware of the consumer’s record and how information becomes part of that record.

Recently I shared about Health Information Exchanges (HIEs) (see my last post). HIEs and Document Imaging can be viewed as two sides of the same coin. HIEs share data electronically without a document ever having to be printed, while Document Imaging is generally an electronic copy of a printed document.
John Mancini, president of the Association for Information and Image Management, has opinions about the insufficiencies of the EHR based on personal experience, as well as his own expert opinion. I love to take exception to an expert opinion, and still I’ve seen tremendous movement toward scanning outside documents into a consumer’s EHR. Most mental health and addictions treatment software manufacturers have or plan to have built in technology to include scanned documents from outside sources like labs and other professionals. They even interface to document imaging systems created for multiple departmental environments like hospitals. I imagine it is common enough for a private practice to rely on the paper chart, and certainly our industry hasn’t become fully acclimated to the EHR. Implementation of the EHR has, however been on the increase, and there’s a deadline. The commandment is for professionals to be operational on the EHR by 2014. Originally envisioned in the Bush era as a primary task that would be nothing but good for healthcare in the United States, this goal was reiterated by president Obama when he took office. Both Document Imaging and HIEs contribute to a consumer’s electronic record.
Along with document imaging capabilities, I commonly see software interfaces to labs and pharmacies required as part of the purchase of an EHR. Interfaces to electronically share data are big business, and can be expensive. Without stimulus funding in the form of Meaningful Use incentives, professional organizations in our industry can lag behind the requirement, simply because they can’t afford it. In our sector of healthcare, some professionals rely less on labs and pharmacies than others, so they may not have enough data volume to justify an interface…in some cases the cost outweighs the benefit. Other professionals may see the value in having the data on the computer, and can’t see that interfacing to these ancillary providers will even be used when they have a printed lab report that all the professionals in the organization are used to.
One thing is certain; searching for a paper document can slow down service for the consumer, and is where document imaging comes in handy.
In a computer, each consumer is assigned a number, and that number is likewise associated with the lab results and pharmacy orders or other document when scanned into the computer’s secure database.
If a consumer comes to a professional with a referral from another facility, or an existing consumer returns with a discharge summary after a stay in the hospital, the associated documentation can be electronically attached to the consumer’s record number, with a link or command button available in the consumer record that pops the lab results or list of currently filled medications to the screen.
My last post discussed how Health Information Exchanges (HIEs), which eliminate the need for a provider to scan and attach these types of data to the consumer’s record by making them available electronically: • Current demographics • Diagnosis treated • Services rendered • Medications prescribed • Admission and Discharge summaries
Whether or not professionals and the organizations they work for will profit from interfaces or HIEs to electronically share data, or be better able to justify a document imaging system, either as an added stand-alone system or one that’s built into their (EHR), is a decision that needs to be made with the consumer’s treatment experience in mind. It’s never a bad idea to chat with a consultant when it comes to determining the better value of multiple technological choices.
Read more → - 13
-
- 07
Jun - (0)
Health Information Exchange
The number one trend in my business, according to Healthcare Technology News will be the growth of Health Information Exchanges (HIE).
We’ve known the importance of electronic sharing of patient data for decades, and these days the hesitancy we felt in the past has become an obsolete emotion. With the advent of HIPAA and its embracement by forward moving legislation as well as new technologies, confidentiality is better assured than ever before.

In mental health and addictions treatment, there are a number of elements of patient data that can be shared that provide a number of benefits. Mistakes are fewer and efficiency is increased on the data entry side of recordkeeping. Treatment can be improved with a broader knowledge of the consumer’s healthcare events and who’s been treating them lately. Conceivably, when a billing address changes, the HIE could assure all professionals in the neighborhood treating the consumer have the most recent information. Professionals have dreamed of having access to few key types of data that multiple agencies treating a consumer might need in order to effectively treat the patient: • Current demographics • Diagnosis treated • Services rendered • Medications prescribed • Admission and Discharge summaries
Now, these elements are available through HIEs..
I am increasingly impacted by the success of HIEs When I was hospitalized a few years ago, and after discharge treated by a couple specialists within the hospital’s network of associates. I was very happy not to have to fill out so many pieces of paper, so somebody else could enter that data into the computer. It was already verified as correct while I was in the hospital, and immediately available to the specialists as soon as I’d signed a Release of Information (ROI).
This is the essential nature of other sorts of consumer data exchange networks, like a Regional Health Information Organization (RHIO). There are many examples as this model is based on a local network of providers….there tend to be a bundle of different solutions where the need seems to support them, and that’s the case with sharing health information. Usually providers pay to become a member of the RHIO, and they will be able to see other local providers’ information like the elements listed above for a specific consumer. I share the opinion of some experts in the field that eventually all these networks will be joined together by the states, and ultimately the feds to finish creating the National Health Record that was mandated back in the Bush era.
I also agree with Adam Gale, president of KLAS, that with all that availability of data we should wonder what it’s being used for…Is the HIE matching patient addresses with their diagnosis in order to sell a list to a major anti-depressant manufacturer? It’s not likely, and that line of questioning is certainly valid for providers joining an HIE.
Conceivably, the value of the access to patient data should exceed the cost of belonging to an HIE. Will the government mandate for all patient care to be recorded in the EHR include the HIE? Testing the wind and laying out an opinion, I’d say it’s a great goal to have the consumer-authorized availability of information among providers, and for the most part that’s happening…it may take a few extra years get the EHRs connected, simply because the technology to make the secure connection, the mapping of the data from an existing EHR to the format needed by the HIE, and other technical concerns add up to a significant price tag.
Read more → - 07
-
- 02
Jun - (0)
Say It With Pictures…
I heard from a fellow in The Netherlands recently, Erwin van der Hout, who has an intriguing product on the market to facilitate better, more constant communication between consumers and professionals. iPicto is an app for the iPhone that enables these folks to communicate via pictograms.

It turns out that folks diagnosed with dementia, autism, and Asperger Syndrome type memory/brain disorders warm up quite nicely to communicating with pictograms, and iPicto seems to be a good tool for this application. I guess the value in this type of communication tool has been known for quite some time. Van der Hout’s product delivers hundreds of expressive pictograms literally to the user’s fingertips, since they hit the iPhone, and the app enables selection of the pictograms for Email communications. In our Email Interview, van der Hout shared that his research indicates success in using pictograms for communications of this type not only in clinical environments, but also for parent/child communications…the books on his website were not in English, and I’m challenged that way, so I can’t personally back him up in this matter. Perhaps if you can read in German, you can check out the link above to his website and comment on his references to help clarify this.
In spite of how that may sound, I’m all for better communication, as long as it meets the patient information security rules we need to live by. Pictogram communication could be quite effective for people with serious mental health issues, and ultimately make a number of people’s lives happier. The pictogram libraries would be uploaded to the iPhone and iPad, and since there are hundreds, they could prove quite expressive and improve such communications between professionals and consumers.
iPicto on the iPad enables storage of larger pictograms, and as a layman, I could envision using this technology in treatment sessions.
Of course, as with any good idea, kinks need to be worked out. Wouldn’t the pictogram Emails look interesting in the consumer’s Electronic Health Record (EHR)? If you save Emails to that system, check out the record to assure the pictogram actually displays once it’s saved…sometimes that sort of thing is lost in the technical translation.
Lately there has been a ton of buzz about apps for your SmartPhone, and recently I shared that it’s getting easier to find apps and methods to increase security on the SmartPhone. I’ve made other excursions into this world, discovering ACHESS, an app for addiction treatment for which the manufacturer shared their security measures, and after talking with the ACHESS manufacturer, the security seemed good for our purposes. The industry is taking steps, and is closer to secure communications between consumers and professionals, as required by a number of rules that are ultimately rooted in HIPAA requirements. At this point, if you plan to engage in consumer/professional communications with iPicto, you’ll need to take your own security measures. A number of solutions are cropping up, and security opinions abound. Among all those claims and the new technology, I continue to make the same suggestion: consult a professional prior to sharing consumer data on a SmartiPhone, even if it’s with the consumer.
Read more → - 02
