-
- 30
Aug - (0)
Joint Efforts
More often than not, joint EHR implementation efforts have failed.
These days, I’m hearing of more successful Electronic Health Record (EHR) purchase and implementation efforts that include several Mental Health agencies. This is a good thing for professionals and consumers on a variety of levels, not the least of which is accurate recording of treatment history, which paints a picture that may guide both professionals and consumers to more successful treatment and a happier life for the consumer.
 The success is significant because several vendors have attempted to make a big splash by selling a single software implementation to multiple agencies in a geographic area, but it seldom goes anywhere.
The success is significant because several vendors have attempted to make a big splash by selling a single software implementation to multiple agencies in a geographic area, but it seldom goes anywhere. Why is that?
I read an article in Behavioral Healthcare Magazine that tackles this subject, and I can expand on their take.
Lynn Duby, CEO of Crisis and Counseling Centers in Augusta, Maine shared that the five agencies joining together for a software purchase had “strong ties”. That’s tough to develop among competitors, and if there’s no unity, success will be limited. In the past, once a mental health or addiction treatment agency made the decision to buy a certain system from a certain vendor, the implementation often did not go well. The major reason for that is that the customer and vendor were simply not on the same page. When an agency buys an EHR, there are a lot of considerations beside price and whatever the driving force is to buy it now…what about the consumer? If professionals are stumbling through the software’s workflow to find the documents they need to make a point in a session, perform an assessment, or collaborate with the consumer on the treatment plan, the consumer is just sitting there, feeling they are wasting time, or worse, living in their disorder. That’s no fun for anybody, and is bad for business. The solution is to purchase software that works for all the parties involved, and the way to do that is to approach the purchase with a plan that’s been successful elsewhere.
The banding together of five agencies to collaborate on an EHR suddenly becomes much more complicated because they work differently. Sure, the state and federal requirements are the same, but the way professionals work differs from agency to agency…that’s what helps give agencies a personality the consumer can feel when they walk in the door. Duby’s comment about “strong ties” tells us that the software must be flexible enough to suit all five agencies’ workflows for all departments, and the professionals need to be flexible, too, in order to use common electronic documents and make the software affordable…Developing five different treatment plans is pretty expensive compared to making a couple minor adjustments on both the software and professional levels. The professionals who were less-than-enthusiastic about new EHR software either took an active role in the software selection, or developed a very Zen attitude: It is what it is.
It seems to be a fact that decision-making by committee is slower than when a single, strong leader is in the picture. When a number of professionals with different ways of working collaborate on an EHR, the committee becomes the decision-making method. I prefer working with a strong leader (or being one), and there are a lot of strong personalities involved in the management-by-committee scenario. Oftentimes, some of these personalities are at odds with one another and managing conflict becomes a major part of the process. I think it’s a great success when an EHR selection can be made in less than a year. Most either take longer or fizzle out entirely (just to give you an idea, it ought to take 90 days or so).
There are a number of methodologies that can be followed to make the most effective use of time and professional resources in the purchase and implementation of an EHR. Sorting out the acceptable methods for both buying and configuring a software system goes much more smoothly once a specific plan is made, and the committee agrees to stick to the plan. Bringing a number of diverse plans together to hammer out what works for all professionals involved is a chore, but without a commonly accepted plan, likelihood of success is diminished.
If you’re involved in a scenario like this, it’s good to have a professional on hand to guide the committee, whether the group hires a full-time project director or gets guidance from a consultant, success is more likely with a good plan.
Read more → - 30
-
- 23
Aug - (0)
Health Home Technology
The guy living on the street, the hopeless alcoholic/drug addict with other diagnosed problems like depression, schizophrenia, bi-polar disorder and whatever else you can throw into the mix, is about to get better.
.jpg) New York is closing applications for agencies to become Health Homes, which means a bundle of improved treatment solutions to focus on our guy mentioned above are about to hit the field. Health Homes at the base level coordinate care for high-usage consumers. The goal is more focused, knowledgeable team treatment.
New York is closing applications for agencies to become Health Homes, which means a bundle of improved treatment solutions to focus on our guy mentioned above are about to hit the field. Health Homes at the base level coordinate care for high-usage consumers. The goal is more focused, knowledgeable team treatment.Our guy needs help from a number of professionals…His addictions need to be dealt with by special professionals in that treatment field. Additionally, medications need to be prescribed by a psychiatrist for his mental disorders. While we’re treating our high-maintenance consumer, let’s add in a psychologist and perhaps an MSW or two to help him overcome Post Traumatic Stress Disorder (PTSD) and find a place to live.
Since this population of consumers seems to continue on the same loop of treatment, people say “None of it works, so why bother?”
That’s the attitude that propagates the growth of this group of folks who have lost hope. They use a ton of services, and don’t get better. Studies have shown that if concerted efforts to coordinate care are implemented, our guy probably will start to recover from all these problems. OK. Fine. So what’s the problem? We have a community of professionals out there who deal with this sort of thing, Medicaid and Medicare likely will pay for the care, so why aren’t these folks getting better.
The answer may be in communication. Assign a case manager to coordinate care in the treatment community and communicate with professionals involved with the consumer, and you deliver the tools so all the professionals know what else is going on with that consumer. Coordinate and communicate to overcome problems with unknown diagnosis and treatment that can lead to drug interaction problems, conflicting therapies, and so on. If a search of a database of Medicare and Medicaid patients numbers (without names) was performed at every intake, and existing treatment was identified, our guy has a chance of recovering through coordinated, effective treatment. This is of great value to Health Homes in coordinating treatment among professionals.
It took me a while, but this is where Information Technology comes in. Any consumer controls outside access to their health information. I envision a checkbox for each provider in the health home the professional belongs to. The consumer agrees or declines sharing the information. Not perfect, because sometimes we’re dealing with consumer paranoia that keeps those things secret, but hey, we’re trying to help.
Here’s what sorts of information would be available to the professionals’ fingertips once an electronic Health Home network of some sort was settled upon:
.jpg) There are a lot of technological details involved, and IT professionals like me enter the picture to help design and implement the details, but this is as decent a solution. It sure beats faxing paper all over the Health Home network. Regional Health Information Networks (RHIOs) and products like Netsmart’s ConnectCare have a head start on delivering secure access to information like this with consumer approval. The difficulty in IT is not the availability of solutions, it’s modifying professional processes and deploying the solutions, integrating these solutions into existing Electronic Health Records (EHRs).
There are a lot of technological details involved, and IT professionals like me enter the picture to help design and implement the details, but this is as decent a solution. It sure beats faxing paper all over the Health Home network. Regional Health Information Networks (RHIOs) and products like Netsmart’s ConnectCare have a head start on delivering secure access to information like this with consumer approval. The difficulty in IT is not the availability of solutions, it’s modifying professional processes and deploying the solutions, integrating these solutions into existing Electronic Health Records (EHRs). The advice is the same as it was when we were kids: don’t do this in your home without supervision.
Read more → - 23
-
- 16
Aug - (0)
GoogleHealth Not So Healthy
It was doomed from the start.
Long ago, but not so far away I researched Google Health . When I checked out the service, it seemed like a great place for my primary care provider and specialists in cardiology or mental health to electronically transfer the records. Demand drives services like this, and in the end, the demand just wasn’t there for Google’s service. Partly because the demand wasn’t there, partially because it takes programming effort for a software company to meet other software companies’ requirements to securely transfer data, the service didn’t make it.
 It takes a special sort of programmer (aka expensive programmer) to develop secure data transfer technology, and security is the key concern when transferring health care data. Software companies are becoming less and less interested in doing this sort of work in the hopes it will pay off, simply because they’ve developed too many programs that didn’t. The Health Level 7 (HL7) format for transferring data is a good one, and really the standard that’s in use today. Most companies have developed this technology. It’s a matter of mapping data from an element in one program to the right spot in another program, say, like from your mental health or addictions professional’s office to Google. The problem is that every time it’s done, there are so many elements to account for in so many different ways, programmers commonly are re-inventing the wheel to get the right data from point A to point B in a secure fashion. It seems every software company approaches this common solution differently. That takes development, and as I shared, development is expensive. Professionals don’t want to spend the money, so data transfer programs, even those based on HL7, don’t get developed.
It takes a special sort of programmer (aka expensive programmer) to develop secure data transfer technology, and security is the key concern when transferring health care data. Software companies are becoming less and less interested in doing this sort of work in the hopes it will pay off, simply because they’ve developed too many programs that didn’t. The Health Level 7 (HL7) format for transferring data is a good one, and really the standard that’s in use today. Most companies have developed this technology. It’s a matter of mapping data from an element in one program to the right spot in another program, say, like from your mental health or addictions professional’s office to Google. The problem is that every time it’s done, there are so many elements to account for in so many different ways, programmers commonly are re-inventing the wheel to get the right data from point A to point B in a secure fashion. It seems every software company approaches this common solution differently. That takes development, and as I shared, development is expensive. Professionals don’t want to spend the money, so data transfer programs, even those based on HL7, don’t get developed.When I originally looked into Google’s service, I didn’t think the electronic sharing of data was even available, so I saw no value. If it was available, it still requires cooperation from other software companies, and getting competitors to cooperate is a tough and expensive task. If electronic data transfer isn’t available for a scheme like storing my health data in a third party location, then I would need to either do some scanning or manual data entry, and I wasn’t (and still am not) up to either. Besides, patient portals are on the horizon. Patient portals are one answer to a new government mandate that healthcare data, like mental health treatment plans, be available to the consumer. It’s much better than printing a book for every patient who wants a copy of their health record.
I use the Veteran’s Administration as my primary healthcare provider, as well as a few clinics, however my cardiologist is special…I go to an outside professional for that. In order to assure the VA’s system is up to date, I get scanned records from the cardiologist, and that’s almost too much work for me. Sometimes the scans just don’t make it to the VA. Shame on me.
By the way, my heart’s healthy and strong like steel, with apparently no danger of heart attack eminent in case you’re interested.
In our world, everybody’s concerned with confidentiality….I wouldn’t want notes from a private therapy session with a professional released to anybody, and that’s a common feeling. This prevailing attitude makes it awfully tough for third party services like Google Health to make it.
Read more → - 16
-
- 09
Aug - (0)
Approaching Electronic Health Record Implementation
“Implementing an EHR may very well be the single largest project you will ever be a part of in your career”.
Believe it. I would add that if your organization’s EHR implementation wasn’t effective, the solution is to take a different look at how it’s done and plan to optimize what you have…read on.
 The statement above came from an announcement of a NIATx presentation I received recently. In the past, the biggest problem standing in the way of effectively and completely implementing an Electronic Health Record (EHR) for Mental Health and Substance Abuse Treatment was a reluctance to spend valuable professionals’ time and energy that’s required to be successful and make the software do what you want it to do. This could apply to any system, really, from a single provider to a large organization with hundreds of users.
The statement above came from an announcement of a NIATx presentation I received recently. In the past, the biggest problem standing in the way of effectively and completely implementing an Electronic Health Record (EHR) for Mental Health and Substance Abuse Treatment was a reluctance to spend valuable professionals’ time and energy that’s required to be successful and make the software do what you want it to do. This could apply to any system, really, from a single provider to a large organization with hundreds of users.There are a number of approaches to getting the same thing done that all revolve around the same thing: Make the software do what the organization needs. I find that if we look at a few elements at a time, and note people who might be appropriate to head up that aspect of the implementation, we’re more likely to have a successful effort than if we try to blast everything out at once, disrupting the work and lives of every professional and treatment of every consumer.
Here are a few ideas to spur some thought, starting with what I think is most important, and then a couple different aspects of the broader view from experts in getting jobs done.
McLeod’s Method: A call this “my” method, simply because it’s part of the system I use.
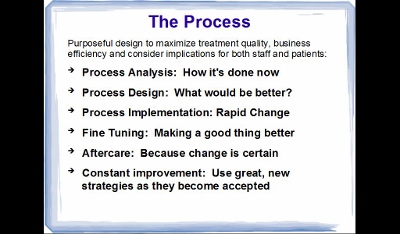 Over the years I’ve picked up a bundle of experience and wisdom from so many sources it would be silly for me to go back and re-construct history….so I call it “mine”. There are many other factors to consider, so I also pay attention to the points attended to by industry leaders in their views below…and more. First, address these bullet points and look into elements like “Rapid-Cycle Change”.
Over the years I’ve picked up a bundle of experience and wisdom from so many sources it would be silly for me to go back and re-construct history….so I call it “mine”. There are many other factors to consider, so I also pay attention to the points attended to by industry leaders in their views below…and more. First, address these bullet points and look into elements like “Rapid-Cycle Change”. Malcomb Baldridge The National Institute of Standards and Technology (NIST) Baldridge Award is a government award for excellence that includes criteria for healthcare for both profit and not for profit organizations. The reason to participate is, according to David Spong, former Boeing executive and winner of the award, is that it improves performance. For professionals, that means not only “production” (seeing more consumers), but improving consumer care for better outcomes. The Baldridge Criteria focus on several elements of importance and help health care organizations achieve and sustain the highest national levels of • Patient safety and loyalty • Health care outcomes • Professional staff satisfaction and engagement • Revenue and market share • Community services
Using the principles and processes of the Baldridge Criteria can’t help but improve an EHR implementation.
NIATx Pointers In a presentation from 2010, NIATx highlighted a number of important points you can use as a guideline in selecting and implementing the EHR. • Why purchase an EHR at all? It may be better for professionals and consumers for the organization to optimize what’s already in place • Is your organization ready? While you’re at it, consider transparency to the consumers and helping them get ready • How do I select a vendor and product? There are tons of approaches: take care, you may want to hire a professional • What about Project Management? Start planning the project prior to purchase so you know what you’re getting into • How does the Implementation affect the entire organization • How do I want to go about training staff and changing business processes to work better for consumers? • What’s the best “Go-Live” strategy? As I’ve said, I’m a big fan of implementing one piece at a time for a bunch of reasons we can talk about later • What are the benefits and problems associated with the EHR implementation?
I don’t mean to sound like a commercial for NIATx, it’s just a good resource. For interested professionals, a NIATx EHR Implementation web presentation is scheduled this week. Given opportunity I plan to listen in, and since I’m a little tardy in posting this, check in with the NIATx website or give them a call to see a copy of the presentation.
Then again, if your organization doesn’t have the people power to manage this sort of effort, and the writing is on the wall that it must be done soon, you may want to consult a professional like yours truly for some help.
Read more → - 09
